Insulin resistance is a stealthy hormone imbalance that can rail-road metabolic health and lead to serious health problems — and it’s on the rise, writes Tania Flack.
Feeling flat and lethargic is a common problem; but imagine if this was happening every day and was only ever temporarily relieved when you gave into your ever-escalating sugar and carbohydrate cravings, only to return with a vengeance an hour later.
Imagine if your weight steadily continued to increase, and no matter what you did belly fat stubbornly accumulated around your middle.
These are just some of the warning signs of insulin resistance, a hormone imbalance that can lead to obesity and diabetes, and increase your risk of other serious health problems like cardiovascular disease, cancer and dementia.
It’s the silent epidemic that no one is talking about in Australia.
READ: Insulin resistance: Are you at risk?
Hypoglycaemia vs insulin resistance
There are two types of blood sugar imbalance.
Hypoglycaemia is caused by temporary drop in blood glucose, which can cause sudden weakness, light-headedness, shakiness, fatigue and mood changes. This is usually easily corrected by eating a nourishing, well-balanced meal and avoiding sugar and refined carbohydrates.
People with hypoglycaemia have reflex surges of insulin; people with insulin resistance, on the other hand, can experience a similar set of symptoms along with constant elevations of insulin, an increase in weight and belly fat.
It is difficult to get an accurate understanding of the prevalence of insulin resistance in Australia, because unlike its more dramatic cousin, type II diabetes, it is not considered a disease, more like a contributing factor to other diseases, so statistics are not officially recorded.
One major sign of insulin resistance is stubborn belly fat and an increase in waist measurement, so if those figures are anything to go by then Australia really is in the midst of a crisis. The Australian Bureau of Statistics reported that in the 2011-2012 period 60.3% of men and 66.6% of women had an unhealthy waist measurement, which indicates an increased risk of insulin resistance.
Insulin is a key regulator of energy metabolism and is pivotal in influencing how the body accumulates and stores fat. When we eat a meal, it is broken down in the stomach and absorbed through the small intestine. Fuel from carbohydrates is converted to glucose and transported around the body in the bloodstream, and then delivered to cells to be used as fuel.
A rise in blood sugar triggers the release of insulin from the pancreas, where it is produced. Insulin acts like a key: it locks onto receptor sites on the surface of cells, which then triggers various intracellular mechanisms that allow the passage of glucose into the cell so it can be used for energy.
Decoding causes
When we eat a meal we absorb more fuel than we can immediately use, so insulin helps to move this extra fuel out of the bloodstream into storage, mainly in the liver, where it is stored in the form of glycogen.
This can be then be easily converted back to glucose when needed. However the liver only has limited storage, and excess glucose will be converted into fat.
Eating foods containing refined carbohydrates and sugar leads to a sharp increase in blood glucose, which causes an increase in fat deposition, predominantly in the intra peritoneal region, creating what is commonly know as dreaded ‘belly fat’. Insulin resistance can also lead to abnormal fat being stored in the liver creating the condition known as ‘fatty liver’, which comes with its own set of health risks.
When we eat a meal high in refined carbohydrates or sugars, we have big rush of glucose, which leads to an abnormally high level of insulin entering the system. Studies show the excessive amount of circulating insulin leads to a reduction in the sensitivity of the insulin receptor sites on the cell.
Insulin resistance occurs when these receptors stop working as well, so while insulin may be readily available it can’t lock onto the receptors as effectively to trigger the transport of glucose into the cell.
People start to feel tired and foggy which triggers sugar cravings, as the cells cry out for more fuel. However, more fuel is not the answer – better transport of the existing fuel is.
This is where the ever-increasing sugar cravings start and the inner war begins: willpower versus the body’s need for energy. It can lead dreadful anguish, as despite all efforts, weight starts to increase and people can feel that they are losing control of their metabolism.
Genetics can play a role in insulin resistance and some people are more likely to develop it than others. However, there are other contributing factors, and often a perfect storm needs to occur for people to develop insulin resistance:
The stress connection Stress can be a driving factor when it comes to insulin resistance, which explains why some people with relatively healthy diets can develop the condition. When we are stressed our body releases a hormone called cortisol, which triggers the release of stored fuel (glycogen) so we have enough energy to fight or flee from danger. This is a vital survival response when we are in actual physical danger. However, cortisol can be triggered by general stress of living in a busy modern world, inflammation, parasitic infection, food allergies, even over-training – the list is endless. So the vicious cycle of stress, increased fuel released into the system, increased insulin, and ultimately insulin resistance begins.
The gut microbiome The impact of imbalanced gut bacteria on metabolism is profound and the subject of extensive research. We know that a high sugar and processed carbohydrate diet leads to an overgrowth in gut bacteria, which is called ‘dysbiosis’. Some of these opportunistic bugs release chemicals, called endotoxins, into the system and these have a low-grade inflammatory effect. This inflammation is thought to directly impact the receptor sites on the cells, making them less efficient and also triggering the release of cortisol, which contributes to insulin resistance via other mechanisms. So addressing gut health can be a crucial step in treating insulin resistance.
Diet This is the cornerstone of treatment when it comes to insulin resistance: a carefully planned diet not only significantly reduces insulin levels but also encourages healthy habits to prevent insulin resistance in the future. A low glycaemic index diet is a good place to start and all processed carbohydrates and sugary foods should be avoided.
Meal timing Interestingly, when we eat is also important in insulin resistance. Six small meals per day was once common advice to anyone wanting to lose weight and balance their blood sugar; however, nothing could be further from the truth. We now know that constantly drip-feeding fuel into our system throughout the day will lead to constant elevations of insulin, which only drives insulin resistance and fuels obesity. We are supposed to rest between meals and have at least one extended fast (overnight) in order to let our body fully process our fuel, store what it can’t use, and reset fully before our next meal. The number one rule in insulin resistance is to eat less frequently!
Natural solutions
Extended overnight fasting is probably the fastest way to reverse insulin resistance as it lowers circulating insulin for extended periods each day, allowing the cells receptors to re-sensitise. It’s ideal for people who need to lose weight, lower inflammation, and rest their digestive system.
This flexible model of fasting works on a sliding time scale. In any one 24-hour period, people fast for 16 hours and can eat two nourishing, well-balanced meals and one healthy snack in the remaining 8 hours. Usually people start their fast at 8 p.m. and end it at noon the following day.
This is ideal for busy people who usually eat on the run in the mornings anyway.
Sadly the average Australian breakfast is high in carbohydrates and sugar and low in nutrients, so missing out is no great loss. It also promotes a mindful approach to food, as people are more likely to plan their two main meals in advance, and it’s a user-friendly way of accessing the benefits of fasting.
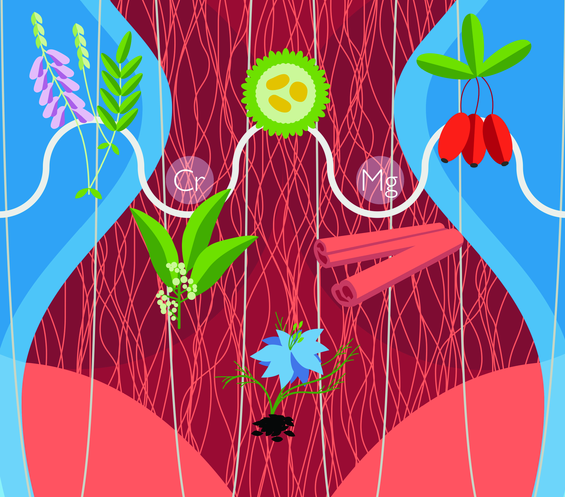
Chromium is a mineral found in trace amounts in many vegetables, whole grains, seafood and meat. Several studies have demonstrated its ability to improve insulin resistance by enhancing the sensitivity of insulin receptor sites.
One double blind, randomised, controlled trial investigated the effects of chromium supplementation on insulin resistance in 85 women with polycystic ovarian syndrome (PCOS). Women who received 1000mcg chromium picolinate daily for six months had significant improvements in insulin levels and reduction in weight. It’s important to note that results only became evident after five months; so longer-term supplementation is needed to get results.
Magnesium is critical for a range of functions in the body – it supports the nervous system and hormone health, and plays an important role in metabolic health. Nuts, seeds, whole grains, legumes and leafy greens are good sources of magnesium, however deficiency is common in Australia.
People with low magnesium are more likely to have insulin resistance and supplementing can reverse this. Best results are seen with regular supplements over a three-month period.
Alpha-lipoic acid is a powerful antioxidant nutrient that has a number of benefits in insulin resistance, not least of which is its ability to improve insulin sensitivity. A clinical trial on a group of type II diabetic patients showed that 600mg of ALA daily, for four weeks, significantly improved insulin sensitivity.
Inositol Much like chromium, inositol has been shown to have significant insulin sensitising effects. One randomised, controlled study involving 44 women with PCOS found that 1200mg per day over six weeks led to a significant improvement in insulin sensitivity.
Many herbs are also beneficial in insulin resistance, including cinnamon, bitter melon, goldenseal, goat’s rue, nigella sativa, and gymnema. Read more about these herbal helpers for insulin resistance.
So if you are losing the blood sugar battle, see your health practitioner. Testing for insulin resistance is easy, and natural medicine, along with the right diet, can really make a difference. Book an appointment today.
This article first appeared in Nature & Health magazine.
Download the article